Fizjoterapia klatki piersiowej kierowana elektryczną tomografią impedancyjną u pacjentów oddziału intensywnej terapii z chorobami płuc: wprowadzenie do metodyki i realizacji w praktyce
Chest physiotherapy guided by electrical impedance tomography in high-dependency unit patients with pulmonary diseases: an introduction of methodology and feasibility
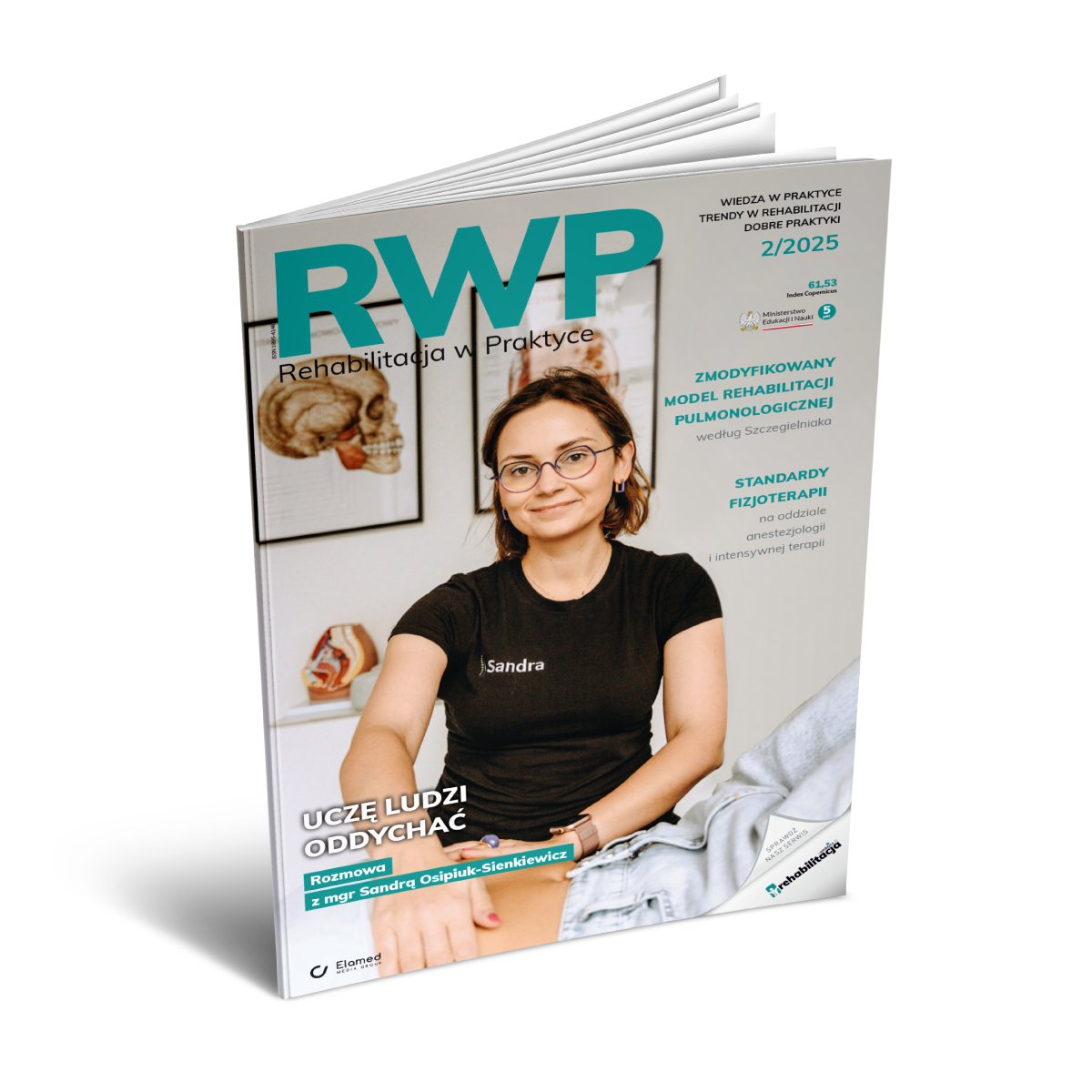
Chest physiotherapy (CPT) has been widely used as an adjunctive treatment to facilitate airway clearance and promote effective coughing (1). Previous studies indicated that CPT could improve lung function and prevent ventilator-associated pneumonia (2). One main challenging issue with current CPT practice is that the objective assessment of ventilation distribution is missing (3). Consequently, the CPT plan is not fully personalized according to individual needs.
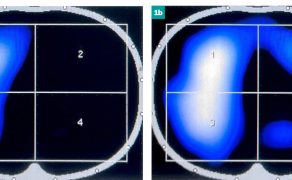
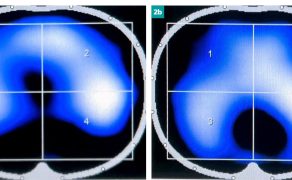
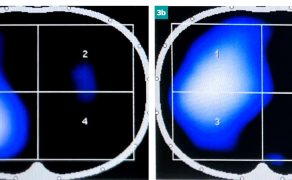
Electrical impedance tomography (EIT) is a radiation-free functional imaging technology that monitors ventilation and perfusion at bedside (4). EIT could potentially provide feedback during CPT to allow its personalized adaptation to individual needs. However, no study has investigated the feasibility to guide CPT using EIT so far.
The aim of the prospective study was to introduce the EIT-guided CPT methodology developed in our center, to analyze its feasibility in patients with airway secretion retention and clearance impairment and to describe feedback from the end-users, both patients and physiotherapists, on its use.
Patients with airway secretion retention and clearance impairment are evaluated for the eligibility of EIT-guided CPT. Untreated pneumothorax and moderate-to-large pleural effusion are contraindications for CPT. In addition, patients with contraindications for EIT measurement are not eligible.
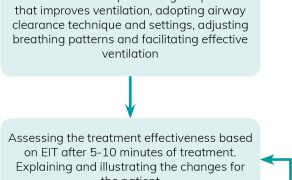
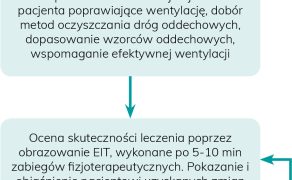
Individualized EIT-guided CPT program is developed for eligible patients. The program consists of 3 parts: (1) understanding of patient’s respiratory status through spatial and temporal ventilation distribution; (2) developing individualized CPT plans accordingly; and (3) evaluating the efficacy and adjusting CPT where necessary. The workflow is illustrated in Fig. 1.
This study was approved by the Ethical committee of Beijing Rehabilitation Hospital (2019bkky-067). Patients with airway secretion retention and clearance impairment admitted to the department from 01.01 to 31.06.2020 were screened.
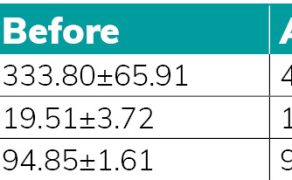
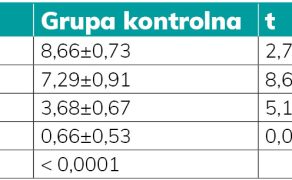
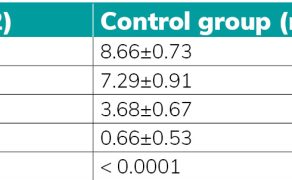
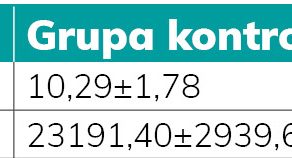
A total of 154 patients were screened for the given period, and 88 were eligible and included. Six patients did not complete the treatment, which corresponded to a dropout rate of 6.8%. Three of them complained about the discomfort of electrode belt application and refused to continue wearing it. The other three patients were not able to cooperate, and the EIT data quality was not good enough for real-time assessment. No adverse events occurred throughout the study.
Galeria
Mogą zainteresować Cię również
Wywiady
„Empatia i doświadczenie – fundament pracy fizjoterapeuty sportowego”. Rozmowa z Wojciechem Hermanem
Jak dużą rolę w profilaktyce urazów odgrywa współpraca między fizjoterapeutami, trenerami przygotowania motorycznego i sztabem medycznym? To na pewno bardzo ważny element, ale nigdy nie uchronisz całej grupy zawodników przed urazami. W obecnych czasach, gdy dynamika gry jest bardzo duża, urazy niestet...